Health Impact News Editor Comments
In the vaccine debate currently raging in modern society, seldom, if ever, is the basic presupposition that vaccines prevent diseases ever questioned. It is assumed by the government and the medical system that this presupposition is a scientific fact.
Without this presupposed “fact”, the justification to force people to receive vaccinations completely falls apart. The acceptance of sacrificing certain children and others due to vaccine harm for “the greater good” also loses its justification, if vaccines actually do not prevent disease. So it is easy to see why those who profit from vaccines, which includes both the manufacturer and the U.S. government, do not want to debate this issue.
What is the actual history and science behind this belief in vaccines? Dr. Viera Scheibner has done everyone a favor in critiquing the current scientific rationale for such a belief, taking a comprehensive look at history and peer-reviewed studies on the subject. We have extracted this from her 50 plus page response to the Australian Academy of Science pro-vaccine report entitled: A critique of the 16-page Australian pro-vaccination booklet entitled “The Science of Immunisation: Questions and Answers” – You can read the entire report here.
We have extracted the relevant information regarding the history and science of vaccines, so that the comprehensive report by Dr. Scheibner can be used by anyone interested in the topic. This is the research you want to print out and give to your doctor if they are uneducated on the facts and science of vaccines. If you are involved in a lawsuit over refusing mandatory vaccines, you will want to give this to your attorney who can enter the information into the court record and start educating judges.
By Dr. Viera Scheibner (PhD)
International Medical Council on Vaccination
Science simply means an organised system of knowledge. It does not mean infallibility, superiority, or eternal validity, and it is subject to changes and revisions. Many a crime has been committed in the name of science, starting with the medieval inquisition, through Nazi Germany’s perversion of just about everything, including medicine, and now, continuing into the present day with harmful excesses of medicine.
In the following [research] I provide documented facts, describing the reality of vaccines/vaccination, as published in reputable peer‐reviewed medical journals.
The documented effects of vaccines as shown by orthodox medical research:
Sensitisation after vaccination.
At the turn of the twentieth century, medical researchers tested vaccines on themselves and other surgeons and medical students and established that vaccine injections result in the so‐called negative phase of lowered bactericidal power of the blood, in other words, a measurable immune‐suppression.(7)
Dr Parfentjev, an employee of Lederle Laboratories (one of many well‐known vaccine manufacturers), reported that vaccination of mice with pertussis vaccine sensitised them, i.e. caused anaphylaxis (as opposed to prophylaxis), and increased their susceptibility to infection with several unrelated species of Gram negative bacteria and viruses.(8)
Sensitisation (anaphylaxis) was achieved with injection of 15 billion cells of commercial pertussis vaccine. Compared with controls (normal, unvaccinated mice) the lethal dose of virus for sensitised mice was much smaller than for normal mice of the same age group. In other words, vaccination with pertussis vaccine increased the susceptibility of mice to lethal shock.
In another benchmark seminal work, Kind demonstrated that pertussis vaccines also sensitised the mice to the lethal effects of subsequent injections of pertussis vaccine as well as a variety of agents and conditions such as anaphylaxis, histamine, serotonin, and endotoxins, and certain proteins of “related” and “unrelated” organisms, such as Escherichia coli and Shigella dysenteriae.(9)
Craighead reported that the same effects as observed in mice were also observed in children given inactivated microbial vaccines. He also wrote that during the past five years, significant advances were made in the understanding of the natural history of a number of common infections, among which he mentioned the apparent states of altered host reactivity consequent to vaccination.
Immunisation with inactivated vaccines could “sensitise” the recipients and result in an accentuated pattern of disease upon natural or experimental exposure.(10)
Meaning, if a child did not react much to the first dose of vaccine, it may react seriously to subsequent doses.
Evidence for delayed hypersensitivity in recipients of “killed” vaccine is demonstrated by local skin reactions after the injection of live or inactivated microorganisms. The dermal response may also be caused by nonmicrobial constituents such as adjuvants and preservatives, which by themselves are highly toxic: aluminium and mercury compounds, formaldehyde, phenol, propylene glycol among others.
Modern immunological research regards vaccines as foreign antigens; indeed, vaccines represent superantigens, which are typified as multiple vaccines administered at the same session.
Earlier researchers have observed the many problems with antigenic stimulation by vaccines, such as the vaccine induced enhancement of viral infections which is known to occur with several vaccines.(11,12) This phenomenon was well described with the failed RSV (Respiratory Syncytial Virus ) vaccines. However, as of 2009, scientists are still unsure of the exact mechanism.(13) As a result, vaccine development for lentivirus infections in general, and HIV/AIDS in particular, has been little successful.(14) Many trials of HIV vaccines, including the latest ones, confirmed this phenomenon: the trials had to be abandoned because a number of human volunteers contracted AIDS from the tested vaccines.
Equally unsuccessful are vaccines against bacterial infections such as whooping cough, diphtheria and Haemophilus influenzae as shown later in this critique.
Sabath documented antigen‐induced transient hypersusceptibility to infections in mice and infants.(15) In mice they determined onset of infection and death due to influenza virus challenge at different times after antecedent monovalent influenza vaccine administration. In infants hospitalised for purulent meningitis there was a clustering of time intervals between routine vaccination and the onset of symptoms, proving the causal link.
Daum demonstrated a decline in serum antibody to the capsule of Haemophilus influenzae type b in the immediate postvaccination period in children.(16) They wrote that this increases the risk of invasive disease if it occurred during a period of asymptomatic colonization with H. influenzae type b, which, of course is a rule rather than an exception, because the bacterium is a ubiquitous commensal living on tonsils.
Effectiveness of vaccination.
Outbreaks and epidemics of measles, whooping cough and poliomyelitis diseases in unvaccinated and fully vaccinated populations.
The Amish are a religious community living across the USA that claim religious exemption to vaccination. Thus, the vast majority are not vaccinated.
They had not reported a single case of measles between 1970 and 1987.(17) At the same time, non‐Amish highly‐vaccinated communities still reported 2‐3 year epidemics. Despite this obvious vaccination failure, pro‐vaccinators claimed success with the measles vaccine.
In 1982, just when the US Secretary of State Joseph A. Califano Jr. planned to announce eradication of measles, the well‐vaccinated non‐Amish populations started reporting huge outbreaks. The unvaccinated Amish did not have large epidemics of measles until much later, starting in early December 1987.
Outbreaks in the fully vaccinated American children continued with increasing frequency and severity. Without disclosing the vaccination status of children in measles epidemics, claiming victory over measles is just empty jabbering.
Moreover, vaccinated children started developing an especially vicious form of atypical measles. Fulginiti described the occurrence of atypical measles in children given formaldehyde‐treated, aluminium precipitated measles vaccine, also referred to as “killed” measles.(18) He explained the problem as due to the altered immunological host response caused by vaccination.
Later on, when live‐attenuated measles vaccine was introduced, the recipients starting developing atypical measles from it, as well.
Rauh and Schmidt described nine cases, which occurred in 1963 during a measles epidemic in Cincinnati.(19) The authors followed 386 children who had received three doses of killed measles virus vaccine in 1961. Of these 386 children, 125 had been exposed to measles and 54 developed it. The authors concluded that:
it is obvious that three injections of killed vaccine had not protected a large percentage of children against measles when exposed within a period of two-and a half years after immunization.
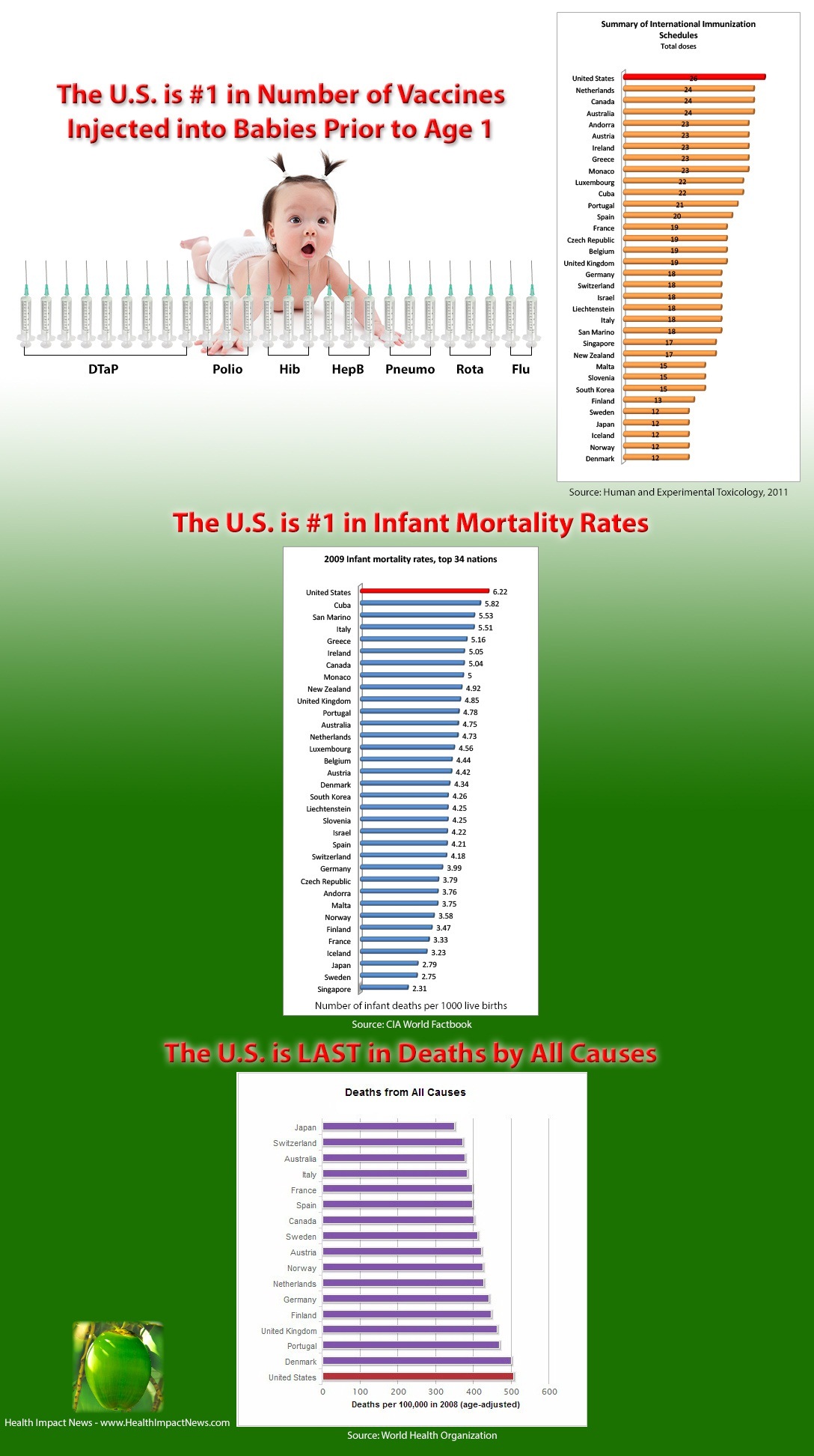
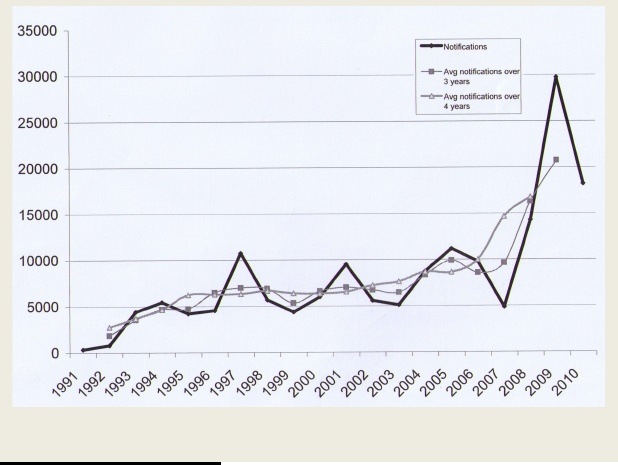
Even when vaccination rates in the UK dropped in the 1990s and early 2000s, when confidence in the vaccine fell, measles deaths never exceeded 4 per year, and remain today at that level. Increasing laboratory‐confirmed measles continue to occur in England and Wales even since vaccination rates have gone back to former levels. (Figure 1.)(20) This is evidence that measles vaccines at best interrupt transmission, but do not confer reliable immunity no matter how much of the herd is vaccinated.
Outbreaks of whooping cough (pertussis) in the vaccination era.
Right after the intense DPT vaccination that started in the mid 1970s, and right through the first decade of 2000, whooping cough outbreaks hit several US states, accompanied by similar outbreaks in all other countries that adopted intensive vaccination including Australia.
In addition to pertussis (and measles) outbreaks in fully‐vaccinated children, the outbreaks in the last thirty‐odd years have been occurring increasingly in very young babies, born to mothers who were vaccinated when they were babies and as a result they lack transplacentally‐transmitted immunity (TTI). Before the vaccine era, TTI protected babies and young children for up to two years against any infectious diseases of childhood.
Lennon and Black demonstrated that hemagglutinin‐inhibiting and neutralizing antibody titers are lower in younger women who have been vaccinated than they are in older women.(21) The same applies to measles and pertussis.(22)
Breastfed infants of vaccinated mothers in the USA have nearly three times the risk of measles infection compared to those of naturally immune mothers, even in the era of vaccination when there is supposedly less measles virus in the environment.
Infants whose mothers were born after 1963 had a measles attack rate of 33%, compared to 12% for infants of older mothers. Infants whose mothers were born after 1963 are more susceptible to measles than are infants of older mothers. An increasing proportion of infants born in the United States may be susceptible to measles. . . the adjusted odds ratio for maternal year of birth (born after 1963) was 7.5 (95% confidence interval 1.8, 30.6).(23)
This is most likely the result of lower levels of virus‐specific immunity in the serum and milk in vaccinated mothers compared to naturally immune mothers. While the overall clinical case rate may have declined with measles vaccination, the most sensitive members of the herd are at an increased risk today‐ because of vaccination.
Hutchins et al. described pertussis epidemiology in the US. They wrote:
During the period 1980-1986, a total of 17,396 cases of pertussis were reported to CDC… The annual incidence of reported pertussis rose from 0.5 cases per 100,000 population to 1.7/100,000. Infants less than 12 months old had the highest average annual incidence… Children 1-4 years of age accounted for 25% of all cases but had an average annual incidence only 1/7th that of infants.(24)
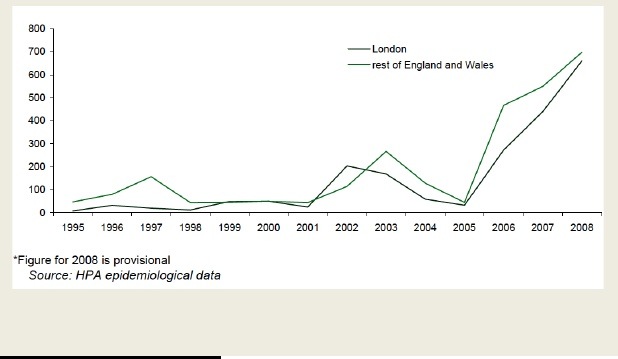
Figure 2 (25) reveals a steady downward trend in the incidence and mortality from pertussis between 1922 and until about 1975‐6; thereafter the downward trend in pertussis morbidity stopped and went sharply upwards, while pertussis mortality remained high but stationary. What could have caused such increase in the disease incidence seen in figure 3?
Hutchins et al. showed the reason for the increase, unwittingly, when they also wrote:
In 1978 a nationwide childhood immunization initiative was begun. Individual States passed legislation requiring proof of immunization for school entry at 5-6 years of age.
The vaccination age started at 6‐8 weeks (and not at 5‐6 years), and large numbers of very young babies were vaccinated within a short period of time; hence the observed major increase of whooping cough in those babies straight after the first dose.
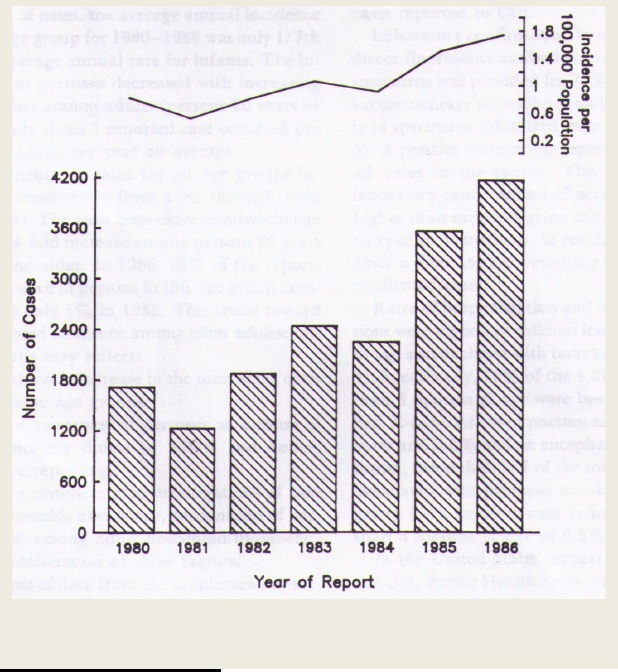
Figure 3: Number of Pertussis Cases Reported to MMWR and Incidence of Disease per 100,000 Population, United States, 1980‐1986.
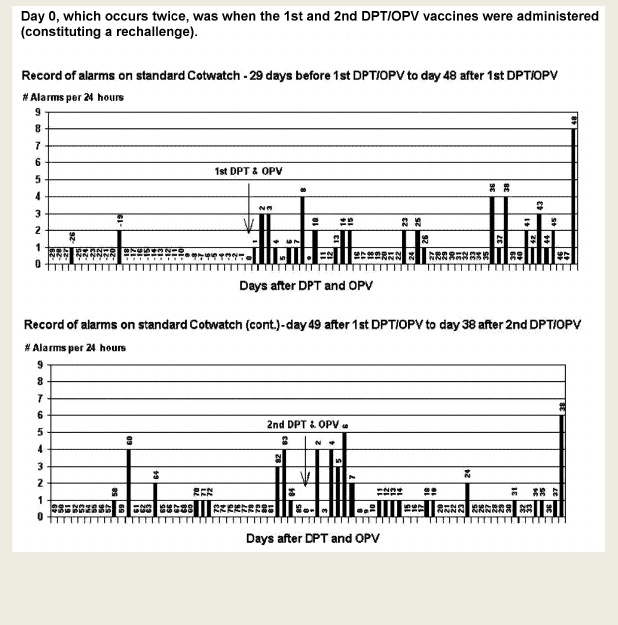
This also coincided with a sudden upsurge in cot deaths, of which the so‐called Tennessee deaths were widely publicised. Bernier(26), Walker(27), and Griffin(28) all described a number of such tragedies. Their data showed a clear clustering of these deaths along the critical days as documented by data collection of babies breathing with Cotwatch breathing monitor.(29)
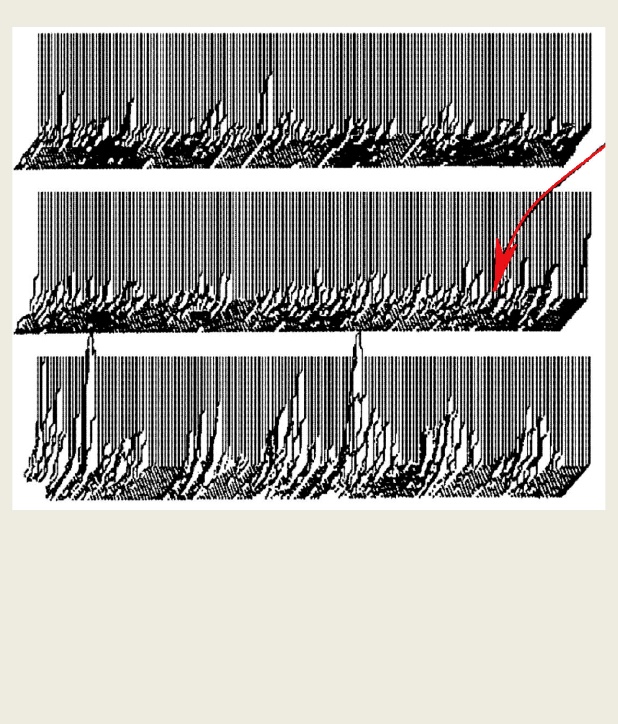
Figure 5: A “raw” record of breathing of baby one, as printed from the microprocessor Cotwatch breathing monitor. Every vertical line represents a histogram of events for one hour. Events from 6 to 15 seconds are mostly apneas (pauses in breathing), while the events above 15 seconds are mostly hypopneas (low volume breathing, which is only 5% of the volume of unstressed breathing). Hypopneas occur at critical hours in clusters of several shorter episodes within 10‐15 minutes and are associated with exposure to a great variety of stressors. The entire record represents 21 days of non‐stop monitoring in sleep. The arrow indicates the day when the DPT vaccine was administered. A marked change in the pattern and duration of events in breathing occurred after the injection.
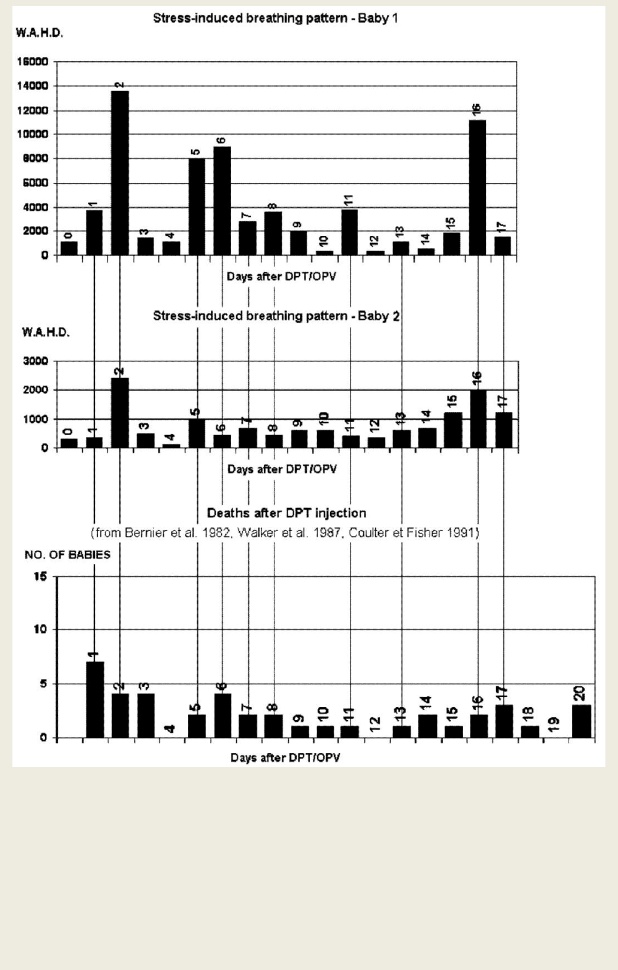
Figure 6: First and second charts: Record of events in breathing in two babies, as printed from the microprocessor Cotwatch breathing monitor. ‐ baby one had been given the third DPTP (diphtheria‐pertussis‐tetanus) and OPV (oral polio) vaccines and ‐ baby two had been give the first DPT and OPV vaccines. Third chart: Actual deaths ‐ 41 randomly listed in deaths in relation to when the last DPT vaccine had been administered.
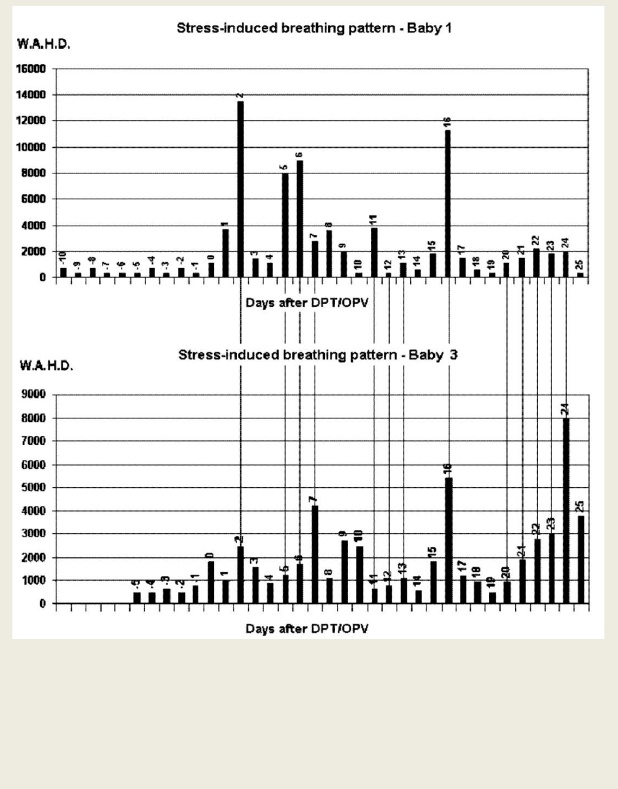
Figure 7: Record of events in breathing in two babies, as printed from the microprocessor Cotwatch breathing monitor ‐ baby one had been given the third DPT (diphtheria‐pertussis‐tetanus) and OPV (oral polio) vaccines ‐ baby three had been given the first DPT and OPV vaccines.
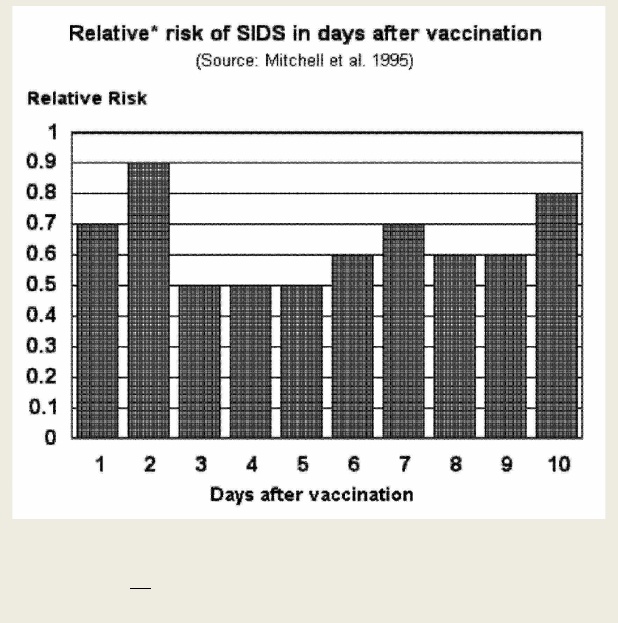
Figure 8: Relative* risk of SIDS in days after vaccination. *Note: The risk is not relative to the risk of SIDS in unvaccinated babies. What is important to note here is the recognisable pattern of critical days.
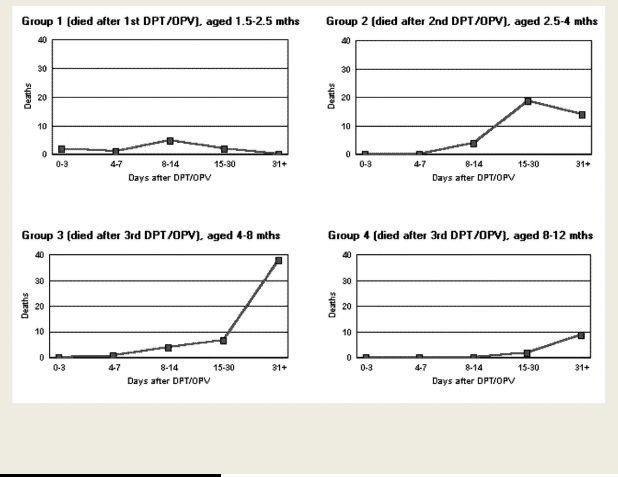
Figure 9: Links age, number of deaths and the time taken to die after vaccination (Source: Griffin et al. 1988)
Due to the 1975 UK television program reporting on brain damage linked to DPT vaccine, the vaccination compliance fell down to 30%, or even 10% in some areas, in the UK. This was followed by the longest inter‐epidemic period with the lowest incidence of whooping cough on record.
Fine and Clarkson wrote:
Though overall pertussis incidence fell in England and Wales subsequent to the introduction of vaccination on a national scale in 1950s, pertussis epidemics have continued to occur regularly every 3-4 years. Since epidemic frequency is a function of the rate of influx of susceptibles, it is suprising that the interepidemic period did not decrease after the 1974 fall in vaccine uptake. One explanation for this paradox may be that pertussis vaccines are more effective in protecting against disease than in protecting against infection.(30)
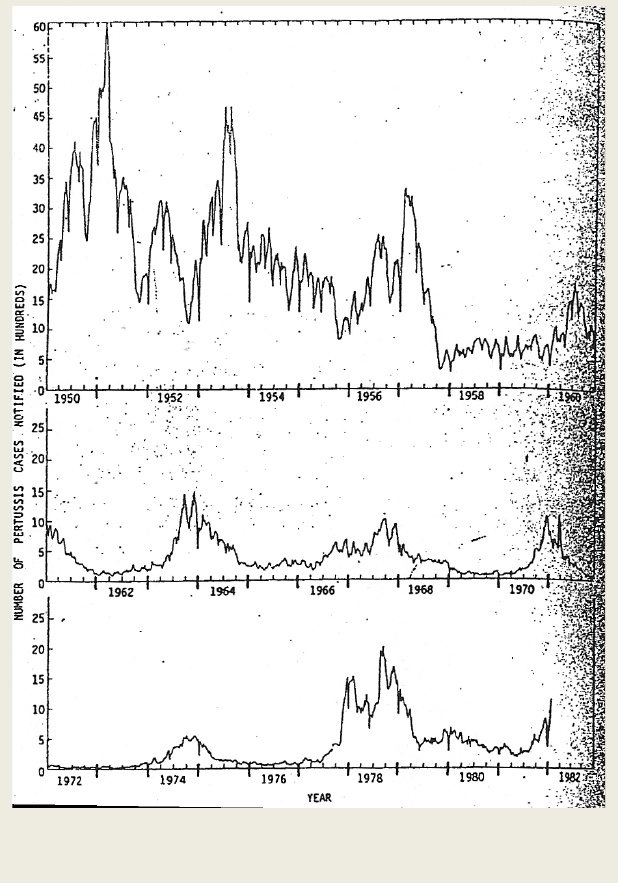
Figure 10: Weekly number of pertussis cases notified to Office of Population Censuses and surveys, from week 1 of 1950 to week 3 of 1982.
It is my opinion that the incidence of whooping cough fell worldwide in the mid 1970s due to natural dynamics, similar to those of measles, and not due to increasing levels of vaccination.
When vaccination stops, the incidence of the targeted disease returns back to normal dynamics. This explanation is supported by another observation in the UK and former West Germany. Miller and Farrington wrote:
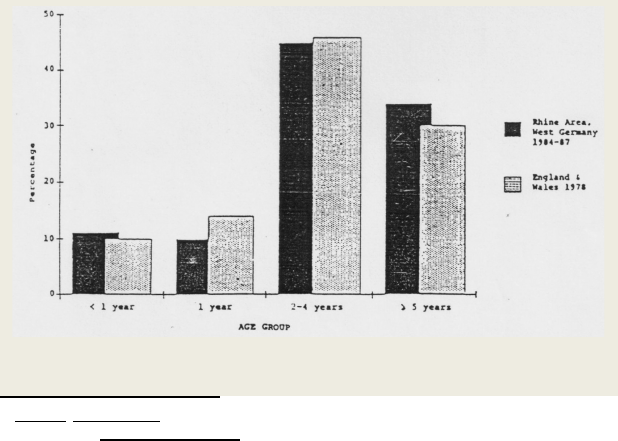
In the West Germany unlike the UK, there are no national statistics on pertussis incidence, no national vaccination policy and no figures for vaccine uptake. . . vaccination rates are low and pertussis is prevalent, particularly in the 2-4 year age group, which is typical of a country with low vaccination uptake; similarly serotype 2 predominates. . . The age distribution was similar to that of cases reported in the UK during 1978 when vaccine uptake was at it’s lowest with the highest proportion occurring in children aged 2-4 years.(31)
Figure 11 (32) is very instructive. The facts point strongly against the presumed benefits of vaccination.
The dynamics of vaccine uptake as described above are also reflected in the dynamics of infant deaths after four weeks in England and Wales. According to Macfarlane:
The postneonatal mortality rate fell markedly in 1976, the year in which a sharp decline in perinatal deaths began. Between 1976 and 1979, however, neither the later neonatal nor the postneonatal mortality rate fell any further. Indeed, the postneonatal mortality rate increased slightly among babies born in 1977.(33) [when the vaccination compliance started climbing up.]
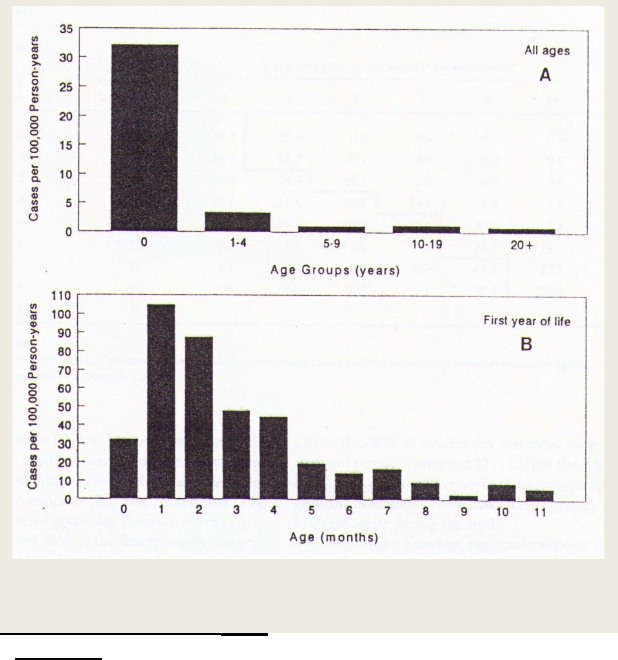
Figure 12: Age‐specific incidence of bacteriologically confirmed pertussis. Massachusetts. 1981‐1991. JID 1994:169 (June)
In contrast, Marchant et al. described inter alia the age incidence of pertussis in Massachusetts in a ten year period 1981‐1991(34) and demonstrated in figure 12 that the highest incidence of bacteriologically‐confirmed pertussis was below the age of one; however, the breakdown in months showed the highest incidence was just after the first and second doses of DPT, with rapid decline afterwards. Equally revealing was the high incidence of pertussis below the vaccination age, in small babies (0 to 6 weeks), this being due to the lack of TTI documentedly caused by the deleterious generational effect of vaccination.(35)
Sutter and Cochi studied pertussis hospitalisations and mortality in the United States between 1985 and 1988 and concluded that there was substantial under‐reporting of pertussis in the US.(36) This of course would have inflated the perceived effectiveness of vaccination. They wrote that based on their indicators, the national health impact of pertussis is considerably higher than previously published reports suggested. Applying the age‐specific hospitalisation rates, 187,867 to 515,930 cases of pertussis may have occurred during the study period, instead of only 14,057 cases reported to the CDC. They concluded that using different methods of estimation, approximately 121,340 cases of pertussis may have occurred during the study period, indicating 11.6% vaccine efficacy. Considering that the pre‐vaccine era pertussis occurrence was in the order of 240,000 cases, vaccination has made no inroads into the pertussis incidence.
Williams et al, made a statement about infants who died:
Infants were less than six weeks of age and died from overwhelming cardiovascular respiratory compromise despite intensive care support. . .The excessive infant mortality from a preventable disease demonstrated the need for better pertussis immunity in the community and for erythromycin treatment of all suspected cases and family contacts.(37)
But, their own data showed something completely different! All four babies were doing OK until they were admitted in hospitals and put on intravenous broad‐spectrum antibiotics. The causal link to the administered antibiotics was clearly shown because the downhill slide followed closely the days when the offending antibiotics were administered.
Moreover, some of the mothers and siblings had whooping cough at the time of the infant’s births, despite being fully vaccinated. One sibling’s vaccination status was uncertain, but he was very likely vaccinated as part of the highly vaccinated generation.
This confirmed two phenomena:
- The increased incidence of whooping cough (and measles) in babies below the vaccination age reflects the lack of transplacentally‐transmitted immunity in the era of vaccinated mothers as predicted by Lennon and Black.(38)
- A well documented phenomenon, that many cases (up to 65%) of infectious diseases develop straight after the first dose of the relevant vaccine in very young children.
Romanus et al. wrote that discontinuation of pertussis vaccination in 1979 in Sweden was followed by a low endemic level of pertussis for 3 years.(39) Thereafter the incidence gradually increased and there were two outbreaks in 1982‐1983 and 1984‐1986. In epidemic years, however, the incidence in infants and small children below the age of one year was very low (11%). The majority of cases (69%) occurred in older children up to 6 years, meaning: when Sweden stopped pertussis vaccination between 1979‐1990, the disease incidence returned back to normal, with most cases occurring at the optimal age.
In contrast to this, when Sweden trialled the acellular pertussis vaccines for the second time (1990‐ 1995), as soon as the trial babies were vaccinated, there was a major outbreak of pertussis in those very young babies.(40) Since 82% of the entire live birth cohort participated in this trial, the pertussis epidemic reached noticeable proportions.
The acellular pertussis vaccine failed to make any inroads into pertussis incidence, as witnessed in Sweden: already during the [second] trials of that vaccine, the infant recipients contracted whooping cough which prompted discontinuation of the trial well before the planned date.(41) This is particularly instructive since during the eleven years without usage of pertussis vaccines (1979‐1990) – babies under one year of age did not contract whooping cough and 90% of cases occurred in the ideal age group between 5‐10 years.(42)
Despite high vaccination compliance, there remained a high persistent level of pertussis in regular 3.5 year epidemics. Vaccines made no inroads into incidence of pertussis as demonstrated in figure 13:
The sordid history of Poliomyelitis vaccination
When the Salk injectable “formaldehyde killed” polio vaccine was tested on some 1.8 million American children in 1954‐55, cases of paralysis in the vaccinated and some of their contacts started occurring within days.(43) The Cutter Laboratories were accused of distributing vaccines containing live polioviruses. Disasters with the Salk vaccines causing vaccine associated paralytic poliomyelitis (VAPP) seem to have been one of the main motivations behind development of an oral “live attenuated” Sabin vaccine, which was believed to simulate the natural infection. However, VAPP cases continued occurring with the Sabin vaccine.
I spent many hours locating and reading the older and more recent articles addressing the effectiveness, or otherwise, of combining IPV and OPV vaccines. I established that the results are not straightforward. Abraham reported that shedding of virulent poliovirus revertants, during immunization with oral poliovirus vaccines, after prior immunization with inactivated polio vaccines, continued.(44) He also documented that prior immunization with EIPV (enhanced potency IPV) does not prevent faecal shedding of revertant polioviruses after subsequent exposure to OPV. (45)
Mensi and Pregliasco wrote:
In recent years great alarm has been generated by outbreaks of paralytic poliomyelitis in vaccinated populations…epidemics were observed in Finland in 1984, Senegal and Brazil in 1986, and Israel and Oman in 1988, all countries in which vaccination is widely deployed. Four epidemics were reported between 1991 and 1992. The first, in 1991, was in Bulgaria, which uses oral vaccination. Forty-three subjects developed paralytic type 1 polio; 88% of them belonged to a normal community and had not completed or even started a vaccination schedule. The second epidemic occurred in The Netherlands, where inactivated polio vaccine (IPV) is used, and involved 68 patients with type 3 poliovirus, members of the Amish…(46) [In The Netherlands they are called members of orthodox religion and in fact use the polio vaccination (compliance between 40‐50% and higher)].
Schaap et al. published a graph (figure 14) correlating the number of reported poliomyelitis cases with the vaccination rates in seven areas in The Netherlands.(47) Interestingly, the areas with the lowest compliance had the lowest number of cases and vice versa. The compliance ranged from 40‐49% to 90‐95%. In the 1992 epidemic, the first two cases occurred in a 14‐year old boy and 23‐year old male nurse, both vaccinated members of the orthodox religious group.
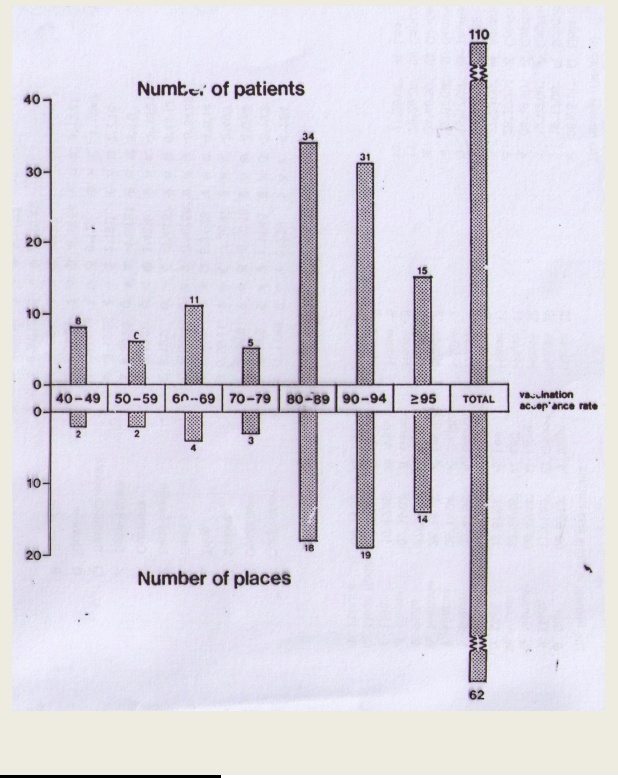
Figure 14: Number of places with polio cases, by average vaccination acceptance rate for birth cohorts 1971‐1975 (Shaap/Bijkerk/Coutinho/Kapsenberg/van Wezel).
Sutter et al described an Oman outbreak as:
. . . evidence for widespread transmission among fully vaccinated children.(48)
Incidence of paralytic disease was highest in children below 2 years:
. . . despite an immunisation programme that recently had raised coverage with 3 doses of oral poliovirus vaccine (OPV) among 12-months-old children from 67% to 87%… with transmission lasting for more than 12 months. Among the most disturbing features of this outbreak was that it occurred in the face of a model immunisation programme and that widespread transmission had occurred in a sparsely populated, predominantly rural setting. (49)
One of the interesting reasons quoted was:
. . . rapid increases in vaccination coverage before the outbreak may have reduced or interrupted endemic circulation of indigenous strains, diminishing the contribution of natural infection to overall immunity levels in the general population. (50)
The same reason was given by Biellik et al. in 1994 when they described the situation in Namibia. They wrote:
Endemic wild poliovirus circulation has continued uninterrupted in Angola and the two northern regions in Namibia across the well-travelled border since 1989, when cases were last reported. Although OPV3 cover age was fairly low in northern compared with southern Namibia, a higher proportion of northern children might have been protected, at least to type 1, by natural immunity, thus suppressing epidemics . . . the apparent interruption of [natural] poliovirus circulation [by vaccination] limited the acquisition of natural immunity. (5)1
Control of polio in the US shows the same phenomenon as the control of pertussis, namely downward trend, which stopped when individual states in the US mandated DPT and polio.
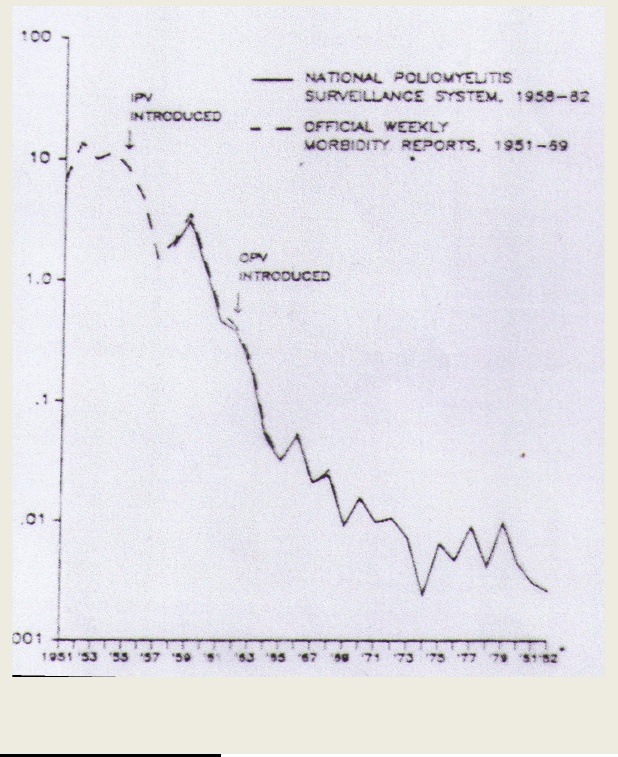
Figure 15: Annual reported paralytic poliomyelitis case rates, United States, 1951‐1982 (Paralytic case rate/100,000 population.) The 1982 data are preliminary.
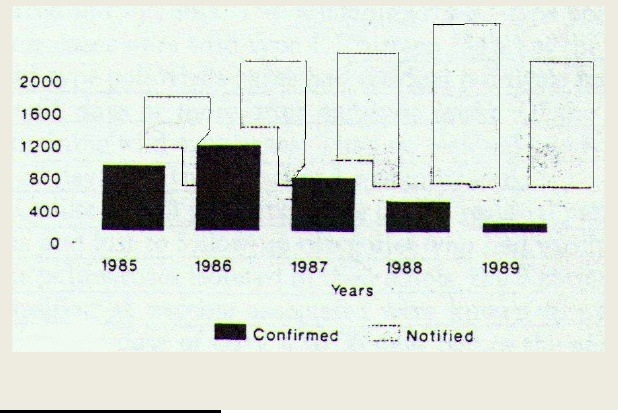
An interesting example of manipulation of data is polio “eradication” in the Americas. Figure 16(52) shows the effect of reclassification of poliomyelitis which allowed the ever increasing number of “notified” cases to morph into an ever decreasing number of “confirmed” cases.
Dr HV Wyatt (53) quoted Hanlon et al. as stating:
…injections during an epidemic may provoke poliomyelitis in children already infected with poliovirus, [and] …provocation poliomyelitis occurs with injections of diphtheria/pertussis/tetanus vaccine, which, I am told, gives rise to unease among vaccinators. The risk of provocation poliomyelitis with the killed poliovaccine…occurred in the Cutter incident.
During a poliomyelitis outbreak in Taiwan, Kim et al. reported that 65% of VAPP developed within 28 days of the first vaccine dose This report confirmed observations of others that two thirds of vaccine‐targeted diseases occur after the first dose of relevant vaccines, including the polio vaccine,(54) and it also unwittingly confirmed the original and true definition of herd immunity that has nothing to do with vaccines: Epidemics occur during the accumulation of two thirds of susceptibles. Once natural immunity is 2/3 of susceptibles get the disease, the epidemic stops. Yet, the authors excluded (as unvaccinated) all paralytic cases (65% of all cases) from calculations of efficacy. Ogra evaluated vaccination with live attenuated and inactivated poliovirus vaccines:
While the combination schedule employing EP-IPV followed by OPV should result in a decline of vaccine-associated (VAP) decease in OPV recipients, such immunization schedule may have little or no impact on the development of VAP in susceptible contacts. Furthermore, the logistics and the cost of combination schedule must be considered before current recommendations based on the use of OPV or EP-IPV alone are revised.(55)
Combined OPV and IPV recommendations
Continuing failures of polio eradication by OPV led to the proposals of using a combination of killed followed by oral polio vaccine delivery. However, such proposals are flawed and based on the ignorance of the documented past experience.
Simian Virus 40 contamination of polio vaccines
Perhaps the worst thing about polio vaccines is their continued contamination by monkey viruses of which SV 40 is the best researched one. According to ample medical research evidence, polio vaccines of any kind cause VAPP. However, there are other major problems with the polio vaccine that justify scepticism about its benefits, one of which is the well‐documented and continuous contamination by monkey viruses SV1‐SV40. Soon after the poliovirus mass vaccination programmes started in the US, a number of monkey viruses and amoebas were found in the vaccine seed brews. Hull, Milner et al. (56) and Hull, Johnston et al. (1955) encountered numerous filterable, transferable cytopathogenic agents other than polio virus in “normal” monkey renal cell cultures. Even though these agents completely destroyed culture tissues, and even caused serious diarrhoea in laboratory animals, all of which died, their possible pathogenesis in humans was ignored or glossed over. The central nervous system was particularly susceptible to the pathogenic properties of such viruses; the histopathological lesions observed in the intracerebrally inoculated monkeys revealed necrosis and complete destruction of the choroid plexus. Findings included generalised aseptic type meningitis. The isolated agent was called simian virus or SV and classified into 4 groups based on the cytopathogenic changes induced in monkey kidney cell cultures infected with these agents.
Hilleman and Sweet (57) reported on the “Vacuolating virus S.V. 40”, which became the best researched among dozens of known monkey viruses. Gerber et al. (58) demonstrated that Sweet and Hilleman’s method of inactivation of SV40 by 10 day treatment using 1: 4000 solution of formaldehyde was inadequate, since it took longer than 10 days to establish that the process was a subject to the asymptotic factor and hence incomplete. Fenner’s research (59) has also established that even the inactivated portion of the viruses reverts back to the original virulence. Dr Bernice Eddy documented the carcinogenic properties of these simian viruses: they caused tumours in hamsters injected with Rhesus monkey kidney cell extracts. (60) As established by many subsequent researchers, in humans SV40 causes characteristic brain tumours, bone sarcomas, mesotheliomas and an especially virulent form of melanoma cancer. The stage was ready for a world‐wide [admitted] contamination of hundreds of millions of children with an oncogenic monkey virus via polio vaccines. SV40 has been directly or indirectly implicated in an epidemic of great number of conditions and brain, lung, bone, renal and other tumours in all ages. (61,62,63,64,65)
Dr Stanley Kops is a modern day advocate for SV40 truth, and he wrote:
To date, the scientific literature and research examining SV40 and cancer-related diseases has been based upon an assumption that SV40 was not present in any poliovirus vaccines administered in the United States and was removed from the killed polio vaccines by 1963. The presumption has been that the regulation for live oral polio vaccine required that SV40 be removed from the seeds and monovalent pools ultimately produced in the manufacturing process…The confirmation of the removal by one manufacturer, Lederle, has been made public at an international symposium in January 1997, where its representatives stated that all Lederle’s seeds had been tested and screened to assure that it was free from SV40 virus. However, in litigation involving the Lederle oral polio vaccine, the manufacturer’s internal documents failed to reveal such removal in all its seeds. The absence of confirmatory testing of the seeds, as well as testimony for SV40 of a Lederle manager indicate that this claim cannot be fully substantiated…(66)
The scientific community should not be content with assurances to the contrary. The continuing occurrence of the above characteristic SV40 tumours in younger and especially quite recent generations of vaccinees should not be ignored or treated with indifference.
Contamination of polio vaccines by chimpanzee coryza virus, or RSV.
Another important consideration in attempts to eradicate poliomyelitis by vaccination is the contamination of polio vaccines by chimpanzee coryza virus, renamed respiratory syncytial virus (RSV).
In 1956, Morris et al. described monkey cytopathogenic agent that produced acute respiratory illness in chimpanzees at the Walter Reed Army Institute of Research and named it chimpanzee coryza virus (CCA). (67)
In 1957, Chanock et al. wrote on the association of a new type of cytopathogic myxovirus with infantile croup. (68)
Chanock and Finberg reported on two isolations of similar agents from infants with severe lower respiratory illness (bronchopneumonia, bronchiolitis and laryngotracheobronchitis). The two viruses were indistinguishable from an agent associated with the outbreak of coryza in chimpanzees (CCA virus) studied by Morris in 1956.
A person working with the infected chimpanzees subsequently experienced respiratory infection with a rise in CCA antibodies during convalescence. They proposed a new name for this agent “respiratory syncytial virus” (RSV). RSV has spread via contaminated polio vaccines like wildfire all over the world and continues causing serious lower respiratory tract infections in infants.
Beem et al. isolated the virus from inpatients and outpatients in the Bob Robert Memorial Hospital for Children (University of Chicago) during the winter of 1958‐1959, in association with human acute respiratory illness. (69) The virus (named Randall) had an unusual cytopathic effect characterised by extensive syncytial areas and giant cells. Soon, 48 similar agents were isolated from 41 patients. There were antigenic similarities between RV and Long and Sue strains of CCA; it produced illness in humans (the age range 3 weeks to 35 years): acute respiratory diseases, croup, bronchiolitis, pneumonia and asthma ranging from mild coryza to fatal bronchiolitis. The isolation rate (46%) was particularly high among infants below six months.
In Australia, Lewis et al. isolated further viral specimens identical with CCA. (70)
Prior to July 1960, the influenza and parainfluenza viruses predominated in infant epidemic respiratory infections; in July 1961 the pattern changed abruptly with sudden increases in bronchiolitis and bronchitis, that were previously infrequent. 58% were under 12 months, and patients under 4 years predominated. Infants with bronchiolitis and severe bronchitis yielded RCA, not previously isolated. Deaths have occurred.
Rogers’ 1959 observations on antibiotic ineffectiveness, and new serious additional problems fell on deaf ears. He wrote that life‐threatening microbial infections continued to occur despite antibiotics, and that the previous microbial landscape also shifted by 1957‐1958. There was streptococcal predominance from 1938‐1940, and then an “impressive” increase in the number of life‐threatening enterobacterial infections post antibiotic.
During the preantimicrobial era most infections were acquired before admission to hospital, while in the postantimicrobial era the vast majority of infections arose in hospital . . . Mycotic infections, especially with Candida albicans, became a major problem. Unusual serious generalised clostridial infections arose and antibiotics have not dramatically altered the risk of, or mortality resulting from, endogenous infections in sick, hospitalised patients. (71)
Levy et al. wrote:
Respiratory syncytial virus (RSV) is the most prevalent cause of lower respiratory tract infections (LRTI) in infants and young children. Infections with RSV is a major health problem during early childhood and primary RSV infections occurs most often between the ages of 6 weeks and 2 years. Approximately one half of all infants become infected with RSV during the first year of life and nearly all infants by the end of their second year of life…in the US each year, approximately 100,000 children are hospitalised at an estimated cost of $300 million. More than half of those admitted for RSV bronchiolitis are between 1 and 3 months of age. (72) [Clearly implicating vaccination.]
RSV vaccine developed in the late 1960s failed miserably. It is no mystery why there is no RSV vaccine recommended today. Fulginiti and others showed the vaccine was ineffective, and induced an exaggerated, altered clinical response… causing RSV illness requiring hospitalisations among vaccinees, and led to delayed dermal hypersensitivity. (73)
Simoes wrote:
Since it was identified as the agent that causes chimpanzee coryza in 1956, and after its subsequent isolation from children with pulmonary disease in Baltimore, USA, respiratory syncytial virus (RSV) had been described as the single most important virus causing acute respiratory-tract infections in children. The WHO estimates that of the 12.2. million annual deaths in children under 5 years, a third are due to acute infections of the lower respiratory tract. Streptococcus pneumoniae, Haemophilus influenzae, and RSV are the predominant pathogens… vaccinated children were not protected from subsequent RSV infection. Furthermore, RSV-naïve infants who received formalin-inactivated RSV vaccine, and who were naturally infected with RSV later, developed more severe disease in the lower respiratory tract than a control group immunized with a trivalent parainfluenza vaccine. (74)
It should surprise nobody that data from ten developing countries — with intense polio vaccination, revealed that RSV was the most frequent cause of LRT infections (70% of all cases).
Polio vaccines are not only ineffective in preventing paralysis, they carry the risk of contamination with many harmful adventitious microorganisms, of which only some monkey viruses have been researched in more detail. Many other potentially dangerous microorganisms remain unaddressed.
Polio vaccination and brain-eating amoebas.
Contamination of monkey kidney tissue cultures (used in the production of polio vaccines) by live amoebas.
In 1996, while watching a TV news report on the death of two 5‐year olds in Australia from brain‐eating amoebae, I remembered a note in Hull et al.’s paper
Recently, an amoeba was isolated from monkey kidney tissue cultures and was identified as belonging to the genus Acanthamoeba. It grew readily in tissue cultures… It appeared to have the ability to infect and kill monkeys and mice following intracerebral and intraspinal inoculation.(75)
Amoebas are unicellular protozoan microorganisms. According to Ma et al.(76), they are classified in the phyllum Sarcomastigophora and belong to Rhizopoda, equipped by propulsive pseudopodia and/or protoplasmic flow without production of pseudopodia. Acanthopodina, a suborder of Amoebida, form two families, Vahlkampfiidae and Acanthoamoebididae, with two genera Naegleria and Acanthamoeba respectively, with a number of species. Naegleria species form three life‐stages, trophozoites, flagellates and cysts and Acanthamoeba species only two, trophozoites and cysts.
Jahnes et al.(77) isolated two strains of apparently the same amoeba which looked like round bodies, similar in appearance to cells manifesting changes induced by certain simian (monkey) viruses. On closer examination, they proved to be amoebic cysts. They varied in size, from 10 to 21 microns in diameter. In one experiment, the cysts were treated with 10% formalin, washed and inoculated into monkey kidney tissue culture tubes. The monkey kidney cells phagocytised the cysts. The trophozooites turned into cysts under refrigeration down to 4 degrees C. These were resistant even under –50 degrees C for months and survived in the pH range 5.0‐9.0. Their tissue cultures were not affected by streptomycin and penicillin.
Culbertson (78,79) confirmed that amoebas caused brain disease and death within days, in monkeys and mice. The reports showed, that following inoculations, “extensive chorio‐meningitis and destructive encephalomyelitis occurred” and killed monkeys in four to seven days and mice in three to four days. Intravenous injections of the amoebas resulted in perivascular granulomatous lesions. Intranasal inoculation in mice resulted in fatal infections in about four days. These mice exhibited ulceration of the frontal lobes of the brain. There were amoebas in the lungs, and they caused severe pneumonic amoeba reaction. Haemorrhage was a common feature. Sections of the kidney showed amoebas present in the glomerular capillaries.
Amoebas showed the ability to migrate through the tissues. The size of the inoculum did not matter: both small and large inoculums produced amoebic invasions. Intragastric inoculations were unsuccessful most probably because amoebic cysts were dissolved by bile.
Researchers, as a rule failed to address the seriousness of the introduction into children of Acanthamoeba via the polio vaccines, even though they were aware of their origin from monkey kidney tissue cultures used in the production of polio vaccines. However they noted that the most contaminated age group was babies below the age of crawling – between 2 and ten months.
Live amoebas were isolated from the air (80) in the UK, together with respiratory syncytial virus, and from the surfaces in hospital cubicles in which infants with acute bronchiolitis were being nursed. The amoebas were isolated at Booth Hall Children’s Hospital in the cubicle occupied by a ten‐week‐old infant with acute bronchiolitis. First, only RSV was isolated and the child sent home, but later an unidentified cytopathic effect was noticed in the tissue cultures and was provisionally called “Ryan virus1” (81) by Pereira, and later also noted in a post‐mortem bronchial swab of another seven‐months old baby boy with RSV bronchiolitis.
Pereira’s paper describes the course of illness: Six days before admission, the baby developed a sore throat and ulcers in the mouth which later spread over the face; he was unwell, could not suck and developed loose stools. The day before admission, he developed a cough and started vomiting. He was drowsy and dyspnoeic, made jerky movements and died soon after admission. Necropsy showed some emphysema, petechiae, and small areas of congestion and alveolar haemorrhaging in the lungs, a fatty liver, prominent mesenteric nodes, and mucopus in the ears. Escherichia coli bacteria were cultured from his ears. Death was diagnosed as due to a respiratory infection associated with encephalomyelitis and hepatitis. Vaccination status was not disclosed, although considering the age, the baby could have received up to three doses of DPT and OPV vaccines.
Armstrong and Pereira identified the Ryan virus as Hartmanella castellanii. (82) They had no doubt that these amoebas came from the human respiratory tract. In Australia, Fowler and Carter(83) Carter(84), and Carter et al.(85) described a number of cases in children and adults. Many cases all over the world occurred in children and adults, with and without histories of swimming in lakes and public swimming pools. (86)
Even if polio vaccines were effective in preventing polio paralysis, their potentially continued contamination by undesirable microorganisms (monkey viruses and amoebas) should encourage the abandonment of their use.
Well‐meaning Rotarians should study the relevant medical research first, before engaging in global polio vaccination.
A critique of the 16-page Australian pro-vaccination booklet entitled “The Science of Immunisation: Questions and Answers” – You can read the entire report here.
Vaccine Epidemic
by Louise Kuo Habakus and Mary Holland J.D.
FREE Shipping Available!
References
7 Wright AE. ON THE CHANGES EFFECTED BY ANTI-TYPHOID INOCULATION IN THEBACTERICIDAL POWER OF THE BLOOD; WITH REMARKS ON THE PROBABLESIGNIFICANCE OF THESE CHANGES. Lancet, Volume 158, Issue 4072, Pages 715 – 723, 14September 1901
8 PARFENTJEV IA. Bacterial allergy increases susceptibility to influenza virus in mice. Proc Soc ExpBiol Med. 1955 Nov;90(2):373-5.
9 KIND LS. Sensitivity of pertussis inoculated mice to endotoxin.. J Immunol. 1959 Jan;82(1):32-7
10 Craighead JE. Disease accentuation after immunisation with inactivated microbial vaccines. J InfectDis. 1975 Jun;131(6):749-54.
11 Ibid. Craighead.
12 Huisman W, Martina BE, Rimmelzwaan GF, Gruters RA, Osterhaus AD. Vaccine-induced enhancement of viral infections.
Vaccine. 2009 Jan 22;27(4):505-12. doi:10.1016/j.vaccine.2008.10.087. Epub 2008 Nov 18.
13 Varga SM. Fixing a failed vaccine. Nat Med. 2009 Jan;15(1):21-2. doi: 10.1038/nm0109-21.
14 Ibid Huisman
15 Sabath et al. Antigen-induced transient hypersusceptibility: a cause of sporadic fulminant infection innormals. 1989. Clin Research; 35(5): 617a
16 Daum RS, Sood SK, Osterholm MT, Pramberg JC, Granoff PD et al.. Decline in serum antibody tothe capsule of Haemophilus influenzae type b in the immediate postvaccinal period. J Pediatr. 1989May;114(5):742-7.
17 Sutter RW, Markowitz LE, Bennetch JM, Morris W, Zell ER, Preblud SR. Measles among the Amish: a comparative study of measles severity in primary and secondary cases in households. J InfectDis. 1991 Jan;163(1):12-6.
18 Fulginiti VA, Eller JJ, Downie AW, Kempe CH. Altered reactivity to measles virus. Atypicalmeasles in children previously immunized with inactivated measles virus vaccines. JAMA. 1967 Dec18;202(12):1075-80.
19 RAUH LW, SCHMIDT R. Measles immunization with killed virus vaccine. Am J Dis Child. 1965Mar;109:232-7.
20 Mellows-Facer A and Thompson G. Measles and MMR statistics – Commons Library Standard Note17 February 2009 | Standard notes SN02581http://www.parliament.uk/briefing-papers/SN02581 accessed 9 Feb 2013.
21 Lennon JL, Black FL. Maternally derived measles immunity in era of vaccine-protected mothers. JPediatr. 1986 May;108(5 Pt 1):671-6.
22 Mulholland K. Measles and pertussis in developing countries with good vaccine coverage. Lancet.1995 Feb 4;345(8945):305-7.
23 Papania M. et al., Increased susceptibility to measles in infants in the United States, Pediatrics, November 1999, Vol. 1045, No. 5, e59, pp. 1-6.
24 Hutchins SS, Cochi SL, Brink EW, Patriarca PA, Wassilak SG et al. Current epidemiology of pertussis in the United States. Tokai J Exp Clin Med. 1988;13 Suppl:103-9.
25 Ibid.
26 Bernier RH, Frank JA Jr, Dondero TJ Jr, Turner P. Diphtheria-tetanus toxoids-pertussis vaccinationand sudden infant deaths in Tennessee. J Pediatr. 1982 Sep;101(3):419-21.
27 Walker AM, Jick H, Perera DR, Thompson RS, Knauss TA. Diphtheria-tetanus-pertussisimmunization and sudden infant death syndrome. Am J Public Health. 1987 Aug;77(8):945-51.
28 Griffin MR, Ray WA, Livengood JR, Schaffner W. Risk of sudden infant death syndrome after immunization with the diphtheria-tetanus-pertussis vaccine. N Engl J Med. 1988 Sep 8;319(10):618-23.
29 Scheibner V. Dynamics of critical days as part of the non-specific stress syndrome discovered duringmonitoring with Cotwatch breathing monitor. 2004 J ACNEM; 23(3): 1-5.
30 Fine PE, Clarkson JA. The recurrence of whooping cough: possible implications for assessment of vaccine efficacy. Lancet. 1982 Mar 20;1(8273):666-9.
31. Miller E, Farrington CP. The current epidemiology of pertussis in the developed world: UK and West Germany. Tokai J Exp Clin Med. 1988;13
32. Ibid.
33 MacFarlane A. Infant deaths after four weeks. Lancet. 1982 Oct 23;2(8304):929-30.
34 Marchant CD, Loughlin AM, Lett SM, Todd CW, Wetterlow LH et al. Pertussis in Massachusetts,1981-1991: incidence, serologic diagnosis, and vaccine effectiveness. J Infect Dis. 1994Jun;169(6):1297-305.
35 Lavine JS, King AA, Bjørnstad ON. Natural immune boosting in pertussis dynamics and the potential for long-term vaccine failure. Proc Natl Acad Sci U S A. 2011 Apr 26;108(17):7259-64.
36 Sutter RW, Cochi SL. Pertussis hospitalizations and mortality in the United States, 1985-1988.Evaluation of the completeness of national reporting. JAMA. 1992 Jan 15;267(3):386-91.
37 Williams GD, Matthews NT, Choong RK, Ferson MJ. Infant pertussis deaths in New South Wales1996-1997. Med J Aust. 1998 Mar 16;168(6):281-3.
38 Ibid. Lennon and Black.
39 Romanus V, Jonsell R, Bergquist SO. Pertussis in Sweden after the cessation of generalimmunization in 1979. Pediatr Infect Dis J. 1987 Apr;6(4):364-71.
40 Olin P. Acellular pertussis vaccines–a question of efficacy. J Hosp Infect. 1995 Jun;30 Suppl:503-7.
41 Ibid. Olin.
42 Isacson et al. 1993. How common is whooping cough in a non-vaccinating country? Pediatr InfectDis J; 12 (4): 284-288.
43 Peterson et al. VACCINATION-INDUCED POLIOMYELITIS IN IDAHO: PRELIMINARYREPORT OF EXPERIENCE WITH SALK POLIOMYELITIS VACCINE. JAMA. 1955;159(4):241-244
44 Abraham R, Minor P, Dunn G, Modlin JF, Ogra PL. Shedding of virulent poliovirus revertantsduring immunization with oral poliovirus vaccine after prior immunization with inactivated poliovaccine.J Infect Dis. 1993 Nov;168(5):1105-9.
45 Carolina Mensi and Fabrizio Pregliasco. Poliomyelitis: Present Epidemiological Situation andVaccination Problems. Clin Diagn Lab Immunol. 1998 May; 5(3): 278–280.
46 Mensi C, Pregliasco F. Poliomyelitis: present epidemiological situation and vaccination problems.. Clin Diagn Lab Immunol. 1998 May;5(3):278-80.
47 Schaap GJ, Bijkerk H, Coutinho RA, Kapsenberg JG, van Wezel AL. The spread of wild poliovirusin the well-vaccinated Netherlands in connection with the 1978 epidemic. Prog Med Virol.1984;29:124–140
48 Sutter RW, Patriarca PA, Brogan S, Malankar PG, Pallansch MA et al. Evidence for widespreadtransmission among fully vaccinated children Lancet. 1991 Sep 21;338(8769):715-20
49 Ibid.
50 Ibid.
51 Biellik RJ, Lobanov A, Heath K, Reichler M, Tjapepua V et al. Poliomyelitis in Namibia. Lancet.1994 Dec 24-31;344(8939-8940):1776
52 De Quadros CA, Andrus JK, Olivé JM, Da Silveira CM, Eikhof RM et al. Eradication of poliomyelitis: progress in the Americas. Pediatr Infect Dis J. 1991 Mar;10(3):222-9.
53 Wyatt HV. Poliovaccination in the Gambia. Lancet. 1987 Jul 4;2(8549):43.
54 Kim-Farley RJ, Rutherford G, Lichfield P, Hsu ST, Orenstein WA, Schonberger LB, Bart KJ, LuiKJ, Lin CC. Outbreak of paralytic poliomyelitis, Taiwan. Lancet. 1984 Dec 8;2(8415):1322–1324.
55 Ogra PL. Comparative evaluation of immunization with live attenuated and inactivated poliovirusvaccines.Ann N Y Acad Sci. 1995 May 31;754:97-107.
56 HULL RN, MINNER JR, SMITH JW. New viral agents recovered from tissue cultures of monkeykidney cells. 1956. Am J Hyg;63:204-215.
57 Sweet, B. H., and M. R. Hilleman. The vacuolating virus, SV40. Proc Soc Exp Biol Med. 1960 Nov;105:420-7.
58 GERBER P, HOTTLE GA, GRUBBS RE. Inactivation of vacuolating virus (SV40) byformaldehyde. Proc Soc Exp Biol and Med; 108: 205-209.
59 Fenner F. Reactivation of Animal Viruses. Br Med J. 1962 July 21; 2(5298): 135–142.
60 EDDY BE, BORMAN GS, BERKELEY WH, YOUNG RD. Tumors induced in hamsters byinjection of Rhesus monkey kidney cell extracts. 1961. Proc Soc Exp Biol and Med; 107; 191-7.
61 Carbone M, Pass HI, Rizzo P, Marinetti M, Di Muzio M et al. Simian virus 40-like DNA sequencesin human pleural mesothelioma. Oncogene. 1994 Jun;9(6):1781-90.
62 Bergsagel DJ, Finegold MJ, Butel JS, Kupsky WJ, Garcea RL.DNA sequences similar to those of simian virus 40 in ependymomas and choroid plexus tumors of childhood. N Engl J Med. 1992 Apr 9;326(15):988-93.
63 Carbone M, Rizzo P, Grimley PM, Procopio A, Mew DJ Simian virus-40 large-T antigen binds p53in human mesotheliomas. Nat Med. 1997 Aug;3(8):908-12.
64 Butel JS and Lednicky JA. Cell and molecular biology of simian virus 40: implications for humaninfections and disease.J Natl Cancer Inst. 1999 Jan 20;91(2):119-34.
65 Weiner LP, Herndon RM, Narayan O, Johnson RT, Shah K Isolation of virus related to SV40 from patients with progressive multifocal leukoencephalopathy. 1972. NEJM;286(8):385-390.
66 Kops, SP. Oral polio vaccine and human cancer: a reassessment of SV40 as a contaminant basedupon legal documents. Anticancer Res. 2000 Nov-Dec;20(6C):4745-9.
67 Blount, R. E., Jr., J. A. Morris, and R. E. Savage. 1956. Recovery of cytopathogenic agent fromchimpanzees with coryza. Proc. Soc. Exp. Biol. Med. 92:544-549.
68 CHANOCK R, FINBERG L. Recovery from infants with respiratory illness of a virus related tochimpanzee coryza agent (CCA). II. Epidemiologic aspects of infection in infants and young children.Am J Hyg. 1957 Nov;66(3):291-300
69 BEEM M, WRIGHT FH, HAMRE D, EGERER R, OEHME M. Association of the chimpanzeecoryza agent with acute respiratory disease in children. N Engl J Med. 1960 Sep 15;263:523-30.
70 Lewis et al.. A syncytial virus associated with epidemic disease of the lower respiratory tract ininfants and young children. 1961. Med J Australia: 932-933 and Forbes (1961. Ibid: 323-325).
71 ROGERS DE. The changing pattern of life-threatening microbial disease. N Engl J Med. 1959 Oct1;261:677-83.
72 Levy BT, Graber MA. Respiratory syncytial virus infection in infants and young children.J Fam Pract. 1997 Dec;45(6):473-81.
73 Fulginiti VA, Eller JJ, Sieber OF, Joyner JW, Minamitani M et al. Respiratory virus immunization. I.A field trial of two inactivated respiratory virus vaccines; an aqueous trivalent parainfluenza virusvaccine and an alum-precipitated respiratory syncytial virus vaccine.Am J Epidemiol. 1969Apr;89(4):435-48.
74 Simoes EA. Respiratory syncytial virus infection.Lancet. 1999 Sep 4;354(9181):847-52.
75 Ibid Hull 1958.
76 Ma P, Visvesvara GS, Martinez AJ, Theodore FH, Daggett PM et al. Naegleria and Acanthamoebainfections: review. Rev Infect Dis. 1990 May-Jun;12(3):490-513.
77 JAHNES WG, FULLMER HM. Free living amoebae as contaminants in monkey kidney tissueculture. Proc Soc Exp Biol Med. 1957 Nov;96(2):484-8.
78 CULBERTSON CG, SMITH JW, MINNER JR. Acanthamoeba: observations on animal pathogenicity. Science. 1958 Jun 27;127(3313):1506.
79 CULBERTSON CG, SMITH JW, COHEN HK, MINNER JR. Experimental infection of mice andmonkeys by Acanthamoeba. Am J Pathol. 1959 Jan-Feb;35(1):185-97.
80 D. Kingston and D. C. Warhurst.. Isolation Of Amoebae From The Air J Med Microbiol February 1969 vol. 2 no. 1 27-36.
81 Pereira MS, Marsden HB, Corbitt G, Tobin JO. Ryan virus: a possible new human pathogen.Br Med J. 1966 Jan 15;1(5480):130-2.
82 J. A. Armstrong and M. S. Pereira. Identification of “Ryan Virus” as an amoeba of the genusHartmannella. Br Med J. 1967 January 28; 1(5534): 212–214.
83 M. Fowler and R. F. Carter.Acute Pyogenic Meningitis Probably Due to Acanthamoeba sp.: aPreliminary Report. Br Med J. 1965 September 25; 2(5464): 734-2, 740-742.
84 Carter RF. Primary amoebic meningo-encephalitis: clinical, pathological and epidemiologicalfeatures of six fatal cases. J Pathol Bacteriol. 1968 Jul;96(1):1–25.
85 Carter RF, Cullity GJ, Ojeda VJ, Silberstein P, Willaert E. A fatal case of meningoencephalitis dueto a free-living amoeba of uncertain identity–probably acanthamoeba sp.Pathology. 1981 Jan;13(1):51-68.
86 Scheibner 1999. Brain-eating bugs: the vaccine connection. Nexus Magazine;(whale.to/vaccines/amoebas.html).