
by Brian Shilhavy
Editor, Health Impact News
Medical professionals from Spain have just published a study (April 2018) on the 13-valent pneumococcal conjugate vaccine (PCV13) that is routinely given to older adults to protect against pneumonia. The study was published in the journal BMC Infectious Diseases.
The PCV13 vaccine has been available since 2012, when it was approved by the FDA. The Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention (CDC) recommends the PCV13 vaccine for persons aged 19–64 years who have high-risk conditions (mainly anatomical or functional asplenia and immunocompromising conditions) and for all persons 65 years or older (with or without risk conditions).
The medical researchers in Spain conducted the study to determine if the vaccine was effective or not in preventing hospitalization from pneumonia.
Benefits using the 13-valent pneumococcal conjugate vaccine (PCV13) in adults are controversial. This study investigated clinical effectiveness of PCV13 vaccination in preventing hospitalisation from pneumonia among middle-aged and older adults.
The study was a population-based cohort study that looked at over two million people over the age of 50 residing in Catalonia, Spain. They looked at both vaccinated and unvaccinated adults, noting those who were hospitalized for pneumonia and those who died from any cause.
The results of their study concluded that not only did the PCV13 vaccine not reduce the risk of pneumonia, it actually increased the risk among those vaccinated.
In this study, the large differences in outcomes between PCV13 vaccinated and unvaccinated suggest that vaccinated persons were sicker.
The study also found that the mortality rate was 60% higher in the vaccinated population (5,944 per 100,000) than in the unvaccinated population (2,354 per 100,000).
Evaluating clinical effectiveness of 13-valent pneumococcal conjugate vaccination against pneumonia among middle-aged and older adults in Catalonia: results from the EPIVAC cohort study
BMC Infectious Diseases Published: 27 April 2018
Abstract
Background
Benefits using the 13-valent pneumococcal conjugate vaccine (PCV13) in adults are controversial. This study investigated clinical effectiveness of PCV13 vaccination in preventing hospitalisation from pneumonia among middle-aged and older adults.
Methods
Population-based cohort study involving 2,025,730 individuals ≥50 years in Catalonia, Spain, who were prospectively followed from 01/01/2015 to 31/12/2015. Primary outcomes were hospitalisation for pneumococcal or all-cause pneumonia and death from any cause. Cox regression models were used to evaluate the association between PCV13 vaccination and the risk of each outcome, adjusting for age, sex and major comorbidities/underlying risk conditions.
Results
Cohort members were observed for a total of 1,990,701 person-years, of which 6,912 person-years were PCV13 vaccinated. Overall, crude incidence rates (per 100,000 person-years) were 82.8 (95% confidence interval [CI]: 77.7–88.1) for pneumococcal pneumonia, 637.9 (95% CI: 599.0–678.7) for all-cause pneumonia and 2367.2 (95% CI: 2222.8–2518.7) for all-cause death. After multivariable adjustments, we found that the PCV13 vaccination did not alter significantly the risk of pneumococcal pneumonia (multivariable-adjusted hazard ratio [mHR]: 1.17; 95% CI: 0.75–1.83; p = 0.493) and all-cause death (mHR: 1.07; 95% CI: 0.97–1.18; p = 0.190), although it remained significantly associated with an increased risk of all-cause pneumonia (mHR: 1.69; 95% CI: 1.48–1.94; p < 0.001). In stratified analyses focused on middle-aged or elderly persons and immunocompromised or immunocompetent subjects, PCV13 vaccination did not appear effective either.
Conclusion
Our data does not support clinical benefits of PCV13 vaccination against pneumonia among adults in Catalonia. It must be closely monitored in future studies involving more vaccinated person-time at-observation.
Leaving a lucrative career as a nephrologist (kidney doctor), Dr. Suzanne Humphries is now free to actually help cure people.
In this autobiography she explains why good doctors are constrained within the current corrupt medical system from practicing real, ethical medicine.
One of the sane voices when it comes to examining the science behind modern-day vaccines, no pro-vaccine extremist doctors have ever dared to debate her in public.
Medical Doctors Opposed to Forced Vaccinations – Should Their Views be Silenced?
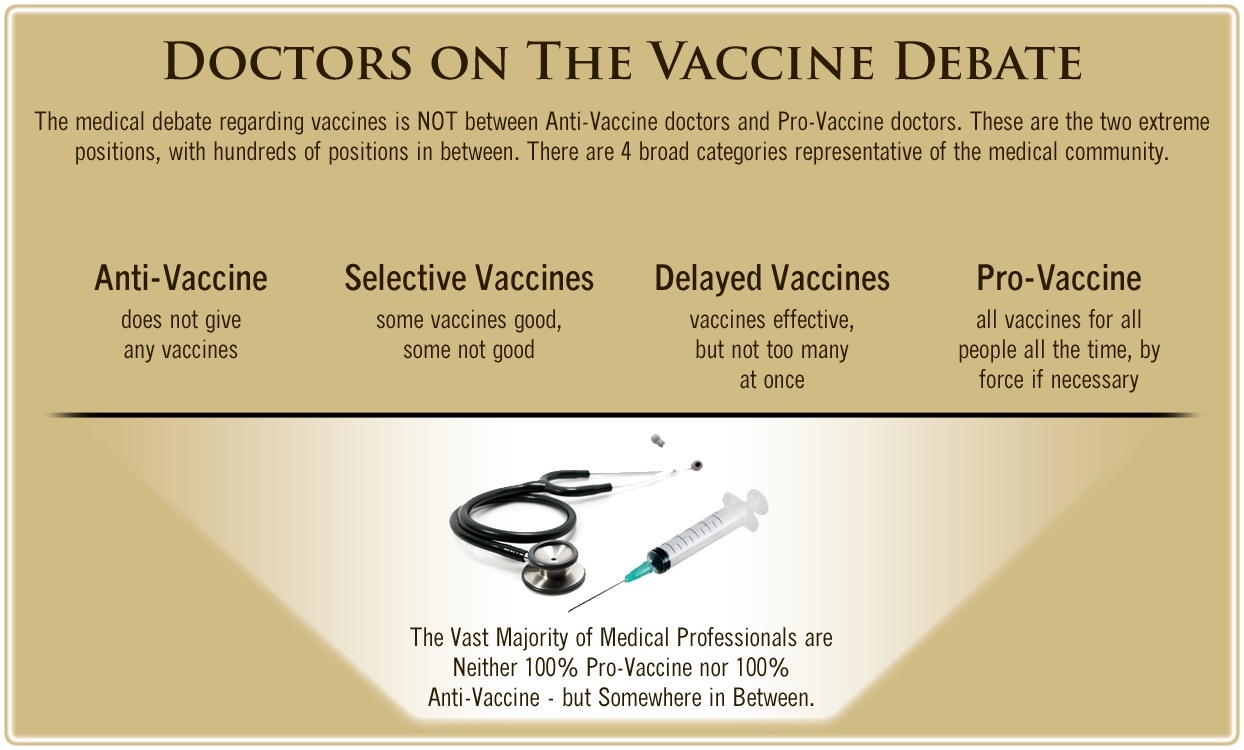
One of the biggest myths being propagated in the compliant mainstream media today is that doctors are either pro-vaccine or anti-vaccine, and that the anti-vaccine doctors are all “quacks.”
However, nothing could be further from the truth in the vaccine debate. Doctors are not unified at all on their positions regarding “the science” of vaccines, nor are they unified in the position of removing informed consent to a medical procedure like vaccines.
The two most extreme positions are those doctors who are 100% against vaccines and do not administer them at all, and those doctors that believe that ALL vaccines are safe and effective for ALL people, ALL the time, by force if necessary.
Very few doctors fall into either of these two extremist positions, and yet it is the extreme pro-vaccine position that is presented by the U.S. Government and mainstream media as being the dominant position of the medical field.
In between these two extreme views, however, is where the vast majority of doctors practicing today would probably categorize their position. Many doctors who consider themselves “pro-vaccine,” for example, do not believe that every single vaccine is appropriate for every single individual.
Many doctors recommend a “delayed” vaccine schedule for some patients, and not always the recommended one-size-fits-all CDC childhood schedule. Other doctors choose to recommend vaccines based on the actual science and merit of each vaccine, recommending some, while determining that others are not worth the risk for children, such as the suspect seasonal flu shot.
These doctors who do not hold extreme positions would be opposed to government-mandated vaccinations and the removal of all parental exemptions.
In this article, I am going to summarize the many doctors today who do not take the most extremist pro-vaccine position, which is probably not held by very many doctors at all, in spite of what the pharmaceutical industry, the federal government, and the mainstream media would like the public to believe.



One Comment