Measles Vaccine Failure: The Glaring Problem Officials Are Ignoring
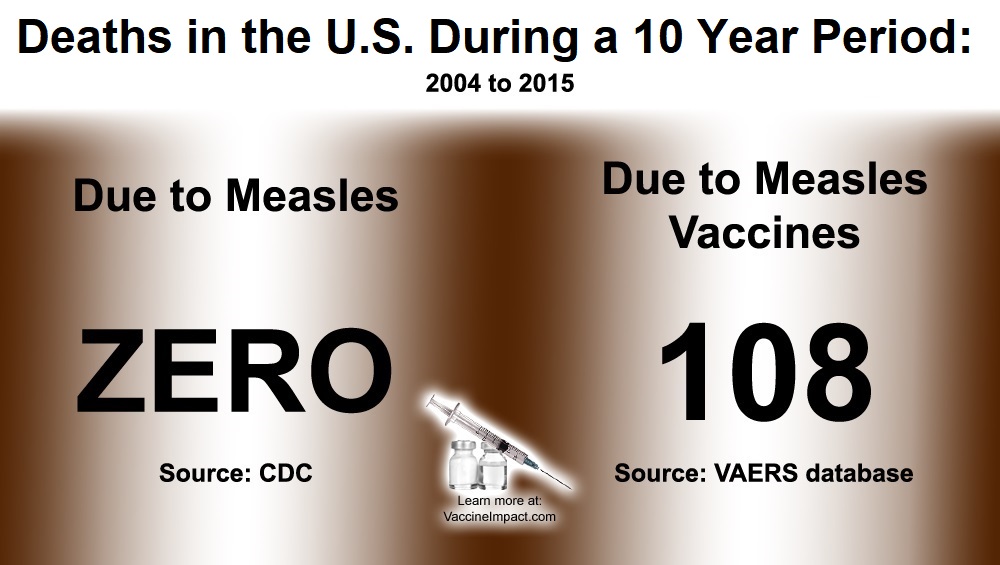
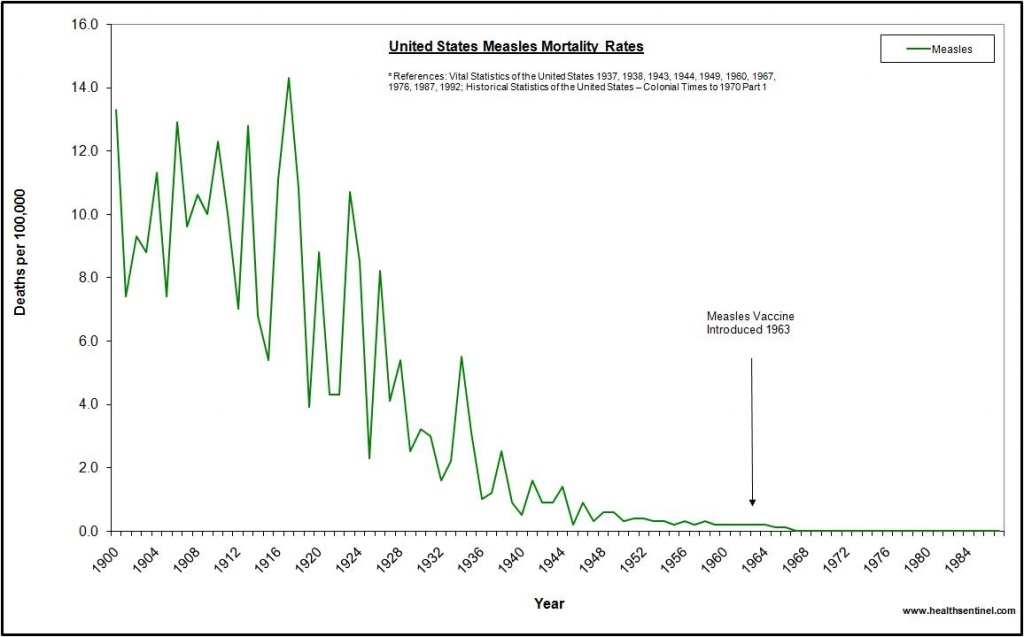
It is far from uncommon for vaccines—including the measles-mumps-rubella (MMR) and MMR-plus-varicella (MMRV) vaccines used in the United States—to fail to live up to their textbook promises. As of 2019, in fact, leading vaccine scientists admitted that “the ability of the current measles vaccine to sustain long-term protective immunity and adequate herd immunity in settings with no wild type virus exposure” is “still a subject of debate.” Right at the starting gate, anywhere from 2% to 12% of children who receive their first measles-containing vaccine exhibit “primary vaccine failure”—defined as vaccine non-responsiveness. For largely unknown reasons, this subset of children (and also adults) fails to mount the expected antibody response after either an initial vaccine or a booster shot. Even in those for whom the vaccine appears to “take,” vaccinated individuals “have lower levels of measles-specific antibody than do those with immunity derived from exposure to wild-type” measles virus. Secondary vaccine failure (waning immunity) is also a built-in feature of measles (and other) vaccines, with vaccine efficacy acknowledged to be “lower and not life-long compared to the wild type virus infection.” Studies show that levels of measles antibody progressively decreasewith increased time since vaccination. Moreover, additional boosters do not solve the problem. In a CDC study of 18-28 year-olds who were given a third dose of MMR vaccine, protection petered out in less than a year—a fact that forced the study’s authors to argue against a routine third dose.